Abstract
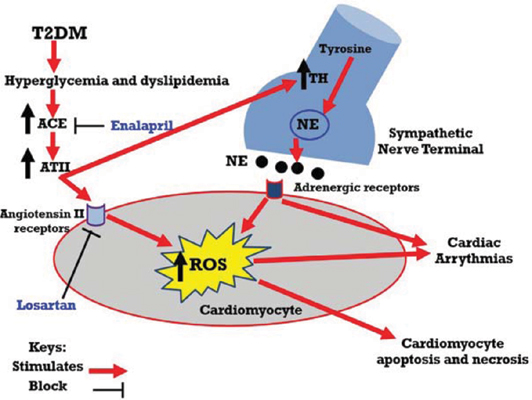
Objective: The present study was designed to investigate the effects of renin angiotensin system (RAS) blockade on cardiac arrhythmias and sympathetic nerve remodelling in heart tissues of type 2 diabetic rats.
Methods: Thirty-two male Sprague Dawley rats were randomly allocated into 4 equal groups; a) normal control group: normal rats, b) DM group; after type 2 diabetes induction, rats received 2ml oral saline daily for 4 weeks, c) DM+ ACEi: after type 2 diabetes induction, rats were treated with enalapril (10 mg/kg, orally for 4 weeks) and d) DM+ ARBs: after type 2 diabetes induction, rats were treated with losartan (30 mg/kg, orally for 4 weeks).
Results: In type 2 diabetic rats, the results demonstrated significant prolongation in Q-T interval and elevation of blood sugar, HOMA-IR index, TC, TGs, LDL, serum CK-MB, myocardial damage, myocardial MDA, myocardial norepinephrine and tyrosine hydroxylase (TH) density with significant reduction in serum HDL, serum insulin and myocardial GSH and CAT. On the other hand, blockade of RAS at the level of either ACE by enalapril or angiotensin (Ag) receptors by losartan resulted in significant improvement in ECG parameters (Q-T), cardiac enzymes (CK-MB), cardiac morphology, myocardial oxidative stress (low MDA, high CAT and GSH) and myocardial TH density.
Conclusion: RAS plays a role in the cardiac sympathetic nerve sprouting and cardiac arrhythmias induced by type 2 DM and its blockade might have a cardioprotective effect via attenuation of sympathetic nerve fibres remodelling, myocardial norepinephrine contents and oxidative stress.
Keywords: Type 2 DM, oxidative stress, diabetic cardiomyopathy, norepinephrine, renin angiotensin system, sympathetic remodelling.
[http://dx.doi.org/10.1111/jdi.12042] [PMID: 23550085]
[http://dx.doi.org/10.1161/CIRCULATIONAHA.106.634949] [PMID: 17242296]
[http://dx.doi.org/10.1111/j.1472-8206.2010.00836.x] [PMID: 20584205]
[http://dx.doi.org/10.1007/s11010-008-9772-y] [PMID: 18425420]
[http://dx.doi.org/10.2478/sjecr-2014-0009]
[http://dx.doi.org/10.1016/S0140-6736(07)60242-6] [PMID: 17416265]
[http://dx.doi.org/10.1016/S0002-9440(10)64598-1] [PMID: 10980124]
[http://dx.doi.org/10.1172/JCI117243] [PMID: 8200970]
[http://dx.doi.org/10.1139/Y11-012] [PMID: 21423295]
[http://dx.doi.org/10.3892/etm.2013.1134] [PMID: 24137228]
[PMID: 11940361]
[http://dx.doi.org/10.1097/00004872-199605000-00015] [PMID: 8762209]
[http://dx.doi.org/10.4103/0976-500X.72350] [PMID: 21350616]
[http://dx.doi.org/10.1590/S0004-28032010000200009] [PMID: 20721461]
[http://dx.doi.org/10.1111/jcmm.12739] [PMID: 26869403]
[http://dx.doi.org/10.1186/s12906-017-1667-6] [PMID: 28288617]
[http://dx.doi.org/10.1002/jsfa.7057] [PMID: 25530163]
[http://dx.doi.org/10.3389/fphys.2018.01669] [PMID: 30534081]
[http://dx.doi.org/10.1093/cvr/cvy226] [PMID: 30184174]
[http://dx.doi.org/10.1016/j.jcjd.2015.09.049]
[http://dx.doi.org/10.4103/bmfj.bmfj_122_18]
[PMID: 29257312]
[http://dx.doi.org/10.1155/2012/217037]
[http://dx.doi.org/10.1016/j.freeradbiomed.2015.11.013] [PMID: 26577173]
[http://dx.doi.org/10.3329/bmrcb.v40i1.20333] [PMID: 26118169]
[http://dx.doi.org/10.1111/jcmm.13252] [PMID: 28643395]
[PMID: 28954833]
[http://dx.doi.org/10.1007/BF02708410] [PMID: 17301496]
[http://dx.doi.org/10.1016/j.bbalip.2009.09.014] [PMID: 19782765]
[http://dx.doi.org/10.1536/ihj.50.627] [PMID: 19809211]
[http://dx.doi.org/10.1016/j.carpath.2017.11.003] [PMID: 29175663]
[http://dx.doi.org/10.2337/db14-0955] [PMID: 25784543]
[http://dx.doi.org/10.1016/j.autneu.2005.05.005] [PMID: 15955747]
[http://dx.doi.org/10.1016/j.ecl.2017.10.010] [PMID: 29407056]
[http://dx.doi.org/10.4239/wjd.v5.i1.17] [PMID: 24567799]
[http://dx.doi.org/10.1016/j.jacc.2004.09.033] [PMID: 15607400]
[http://dx.doi.org/10.2478/sjecr-2018-0049]
[http://dx.doi.org/10.3317/jraas.2001.016] [PMID: 11881114]
[http://dx.doi.org/10.1016/j.bcp.2017.07.022] [PMID: 28789938]
[http://dx.doi.org/10.1161/CIRCULATIONAHA.104.510461] [PMID: 15897343]
[http://dx.doi.org/10.1111/j.1463-1326.2011.01535.x] [PMID: 22074122]
[http://dx.doi.org/10.1007/s11883-011-0214-z] [PMID: 22037772]
[http://dx.doi.org/10.1210/en.2007-1646] [PMID: 18450963]
[http://dx.doi.org/10.1042/CS20110284] [PMID: 21861845]
[http://dx.doi.org/10.1186/1475-2840-6-26] [PMID: 17903269]
[http://dx.doi.org/10.1016/j.febslet.2004.09.027] [PMID: 15498586]
[http://dx.doi.org/10.1038/hr.2010.99] [PMID: 20535122]
[http://dx.doi.org/10.1002/iub.1190] [PMID: 23893738]
[http://dx.doi.org/10.1291/hypres.27.457] [PMID: 15302981]
[http://dx.doi.org/10.7326/0003-4819-122-2-199501150-00010] [PMID: 7992988]
[http://dx.doi.org/10.1016/S0002-9149(03)00432-6] [PMID: 12818733]
[http://dx.doi.org/10.1016/S1262-3636(07)70146-5] [PMID: 15671918]
[http://dx.doi.org/10.1016/S0895-7061(03)00054-2] [PMID: 12745201]
[http://dx.doi.org/10.3904/kjim.2015.404] [PMID: 28490725]
[http://dx.doi.org/10.1097/WOX.0b013e3182439613] [PMID: 23268465]