Abstract
Background: Transcatheter arterial chemoembolization (TACE) is an effective treatment for hepatocellular carcinoma (HCC), however, the complications of TACE have gradually become a concern of clinicians. Injury to the bile duct has been the focus of many scholars.
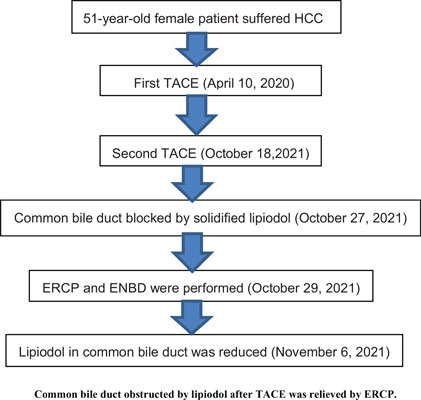
Case Presentation: HCC was diagnosed in a 51-year-old female patient, and the first TACE was performed on April 10, 2020. The second TACE was performed on October 18, 2021. After the second TACE, The patient suffered from nausea, jaundice, and body itching. Computed tomography (CT) of the abdomen showed that the lower common bile duct was obviously blocked by the solidified lipiodol accompanied by dilatation of intrahepatic and extrahepatic bile ducts on October 27, 2021. Endoscopic retrograde cholangiopancretography (ERCP) and endoscopic nasobiliary drainage (ENBD) were performed on October 29, 2021. The deposition of lipiodol in the common bile duct was significantly reduced.
Conclusion: After the transcatheter arterial chemoembolization for hepatocellular carcinoma, we should be on alert for damage to the bile duct, and pay attention to the deposition of lipiodol in the common bile duct.
Keywords: Common bile duct obstructed, lipiodol, transcater arterial chemoembolization, hepatocellular carcinoma, ENBD, computed tomography (CT).
[http://dx.doi.org/10.2478/raon-2021-0047] [PMID: 34957733]
[http://dx.doi.org/10.1007/s12072-022-10423-7] [PMID: 36271176]
[http://dx.doi.org/10.14000/j.cnki.issn.1008-1704.2004]
[http://dx.doi.org/10.1053/j.gastro.2006.05.021] [PMID: 16890600]
[http://dx.doi.org/10.1186/s12957-021-02401-4] [PMID: 34598689]
[http://dx.doi.org/10.1159/000515865] [PMID: 33946070]
[http://dx.doi.org/10.1055/a-1260-2874] [PMID: 33003220]
[http://dx.doi.org/10.1002/rcr2.678] [PMID: 33117542]
[http://dx.doi.org/10.1111/hepr.13620] [PMID: 33462925]
[http://dx.doi.org/10.1111/hepr.12071] [PMID: 23387506]
[http://dx.doi.org/10.1097/00004836-200105000-00013] [PMID: 11319315]