Abstract
Background: Little is known about the efficacy of programmed cell death protein-1 (PD-1) or programmed cell death-ligand 1 (PD-L1) inhibitors in patients with central nervous system (CNS) metastases.
Objective: This study aimed to assess the difference in efficacy of PD-1 or PD-L1 inhibitors in patients with and without CNS metastases.
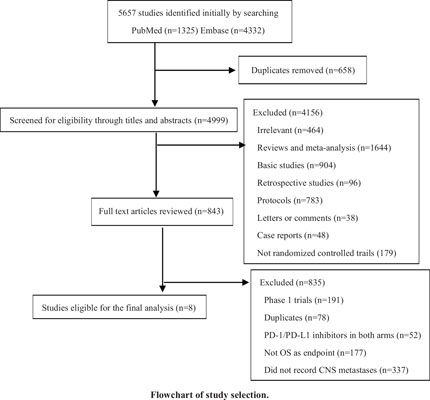
Methods: From inception to March 2020, PubMed and Embase were searched for randomized controlled trials (RCTs) about PD-1 or PD-L1 inhibitors. Only trails with available hazard ratios (HRs) for overall survival (OS) of patients with and without CNS metastases simultaneously would be included. Overall survival hazard ratios and their 95% confidence interval (CI) were calculated, and the efficacy difference between these two groups was assessed in the meantime.
Results: A total of 4988 patients (559 patients with CNS metastases and 4429 patients without CNS metastases) from 8 RCTs were included. In patients with CNS metastases, the pooled HR was 0.76 (95%CI, 0.62 to 0.93), while in patients without CNS metastases, the pooled HR was 0.74 (95%CI, 0.68 to 0.79). There was no significant difference in efficacy between these two groups (χ2=0.06 P=0.80).
Conclusion: With no significant heterogeneity observed between patients with or without CNS metastases, patients with CNS metastases should not be excluded in the PD-1 or PD-L1 blockade therapy. Future research should permit more patients with CNS metastases to engage in PD-1 or PDL1 blockade therapy and explore the safety of PD-1 or PD-L1 inhibitors in patients with CNS metastases.
Keywords: Central nervous system metastases, PD-1/PD-L1 inhibitors, immunotherapy, overall survival, programmed cell death, cell carcinoma.
[http://dx.doi.org/10.1038/nrc.2016.36] [PMID: 27079802]
[http://dx.doi.org/10.1056/NEJMoa1709684] [PMID: 28889792]
[http://dx.doi.org/10.1056/NEJMoa1809697] [PMID: 30280658]
[http://dx.doi.org/10.1056/NEJMoa1510665] [PMID: 26406148]
[http://dx.doi.org/10.1056/NEJMoa1602252] [PMID: 27718784]
[http://dx.doi.org/10.1093/neuonc/nox077] [PMID: 28444227]
[http://dx.doi.org/10.1038/nri3265] [PMID: 22903150]
[http://dx.doi.org/10.1155/2013/512684] [PMID: 24489576]
[http://dx.doi.org/10.1159/000446338] [PMID: 27260656]
[http://dx.doi.org/10.1038/s41572-018-0055-y] [PMID: 30655533]
[http://dx.doi.org/10.1056/NEJMoa1507643] [PMID: 26412456]
[http://dx.doi.org/10.1056/NEJMoa1809064] [PMID: 30280641]
[http://dx.doi.org/10.1038/nature14432] [PMID: 26030524]
[http://dx.doi.org/10.1038/s41593-018-0227-9] [PMID: 30224810]
[http://dx.doi.org/10.1158/1078-0432.CCR-15-1836] [PMID: 27245829]
[http://dx.doi.org/10.1093/jnci/djt276] [PMID: 24108809]
[http://dx.doi.org/10.3171/2013.3.JNS122226] [PMID: 23621605]
[http://dx.doi.org/10.1200/JCO.19.03136] [PMID: 32150489]
[http://dx.doi.org/10.1371/journal.pmed.1000100] [PMID: 19621070]
[http://dx.doi.org/10.1371/journal.pmed.1000097] [PMID: 19621072]
[http://dx.doi.org/10.1136/bmj.d4002] [PMID: 21784880]
[http://dx.doi.org/10.1016/j.lungcan.2018.12.017] [PMID: 30642441]
[http://dx.doi.org/10.1056/NEJMoa1910231] [PMID: 31562796]
[http://dx.doi.org/10.1016/S0140-6736(19)32222-6] [PMID: 31590988]
[http://dx.doi.org/10.1016/S1470-2045(19)30689-8] [PMID: 31786121]
[http://dx.doi.org/10.1016/S1470-2045(19)30689-8] [PMID: 31786121]
[http://dx.doi.org/10.1080/08830185.2017.1357719] [PMID: 28961037]
[http://dx.doi.org/10.7150/thno.40783] [PMID: 32194848]
[http://dx.doi.org/10.1186/s13046-019-1426-2] [PMID: 31623643]
[http://dx.doi.org/10.1080/2162402X.2015.1057388] [PMID: 26942067]
[http://dx.doi.org/10.1016/j.ccell.2017.02.009] [PMID: 28292436]
[http://dx.doi.org/10.18632/oncotarget.22110] [PMID: 29262592]
[http://dx.doi.org/10.1158/1078-0432.CCR-10-1564] [PMID: 20829328]
[http://dx.doi.org/10.1111/his.12537] [PMID: 25314639]
[http://dx.doi.org/10.1016/j.molmed.2014.10.009] [PMID: 25440090]
[http://dx.doi.org/10.1016/j.radonc.2018.08.025] [PMID: 30241791]
[http://dx.doi.org/10.1016/S1470-2045(12)70090-6] [PMID: 22456429]
[http://dx.doi.org/10.1016/S1470-2045(16)30053-5] [PMID: 27267608]
[http://dx.doi.org/10.1186/s40425-018-0336-8] [PMID: 29618381]
[http://dx.doi.org/10.1001/jamaoncol.2018.5904] [PMID: 30605213]
[http://dx.doi.org/10.1016/S1470-2045(18)30261-4] [PMID: 29778737]
[http://dx.doi.org/10.1136/bmj.k3529] [PMID: 30201790]
[http://dx.doi.org/10.1080/2162402X.2020.1746113] [PMID: 32313724]
[http://dx.doi.org/10.1002/cncr.29082] [PMID: 25336142]