Abstract
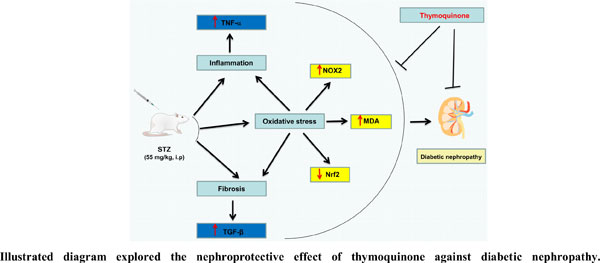
Objective: Diabetic nephropathy is an unavoidable complication of chronic uncontrolled diabetes mellitus. The pathogenesis of diabetic nephropathy is multifactorial, and the development of an effective therapy remains to be elucidated. The aim of the present study was to assess the role of NOX2 and Nrf2 in the protective mechanism of thymoquinone (THQ) against streptozotocin (STZ)-induced diabetic nephropathy.
Methods: Rats were injected with STZ (55 mg/kg) to induce diabetes. The diabetic rats were orally treated with THQ (10 mg/kg/day) for eight weeks.
Results: STZ-treated rats exhibit an elevation of serum creatinine, serum urea, and creatinine clearance. The renal abnormalities were associated with increased NADPH oxidase isoform, NOX2 protein expression, and activity, along with elevated malondialdehyde (MDA). In addition, the tumor necrotic factor-alpha (TNF-α) level and nitric oxide (NO) bioavailability, as well as the transforming growth factor-beta (TGF)-β, were markedly increased. On the other hand, the nuclear factor-E2-related factor (Nrf2) protein expression was significantly reduced in diabetic rats compared to the control. However, treatment with THQ significantly reversed these alterations with subsequent ameliorating renal dysfunction and pathological abnormalities.
Conclusion: The present study demonstrates that THQ could protect against STZ-induced diabetic nephropathy by modulating the Nrf2/NOX2 signaling pathway.
Keywords: Diabetic nephropathy, thymoquinone, oxidative stress, NOX2, Nrf2, TNF-α.
[http://dx.doi.org/10.1155/2021/1497449] [PMID: 34307650]
[http://dx.doi.org/10.1016/j.freeradbiomed.2017.12.040] [PMID: 29305106]
[http://dx.doi.org/10.1016/j.biopha.2018.05.130]
[http://dx.doi.org/10.1016/j.mce.2012.11.004] [PMID: 23174757]
[http://dx.doi.org/10.5582/bst.2011.v5.4.173] [PMID: 21914953]
[http://dx.doi.org/10.1016/j.ejphar.2014.10.021] [PMID: 25446917]
[http://dx.doi.org/10.3181/0705-MR-134] [PMID: 18156300]
[http://dx.doi.org/10.1152/physrev.00018.2001] [PMID: 11773609]
[http://dx.doi.org/10.1016/j.biocel.2020.105851] [PMID: 32949687]
[http://dx.doi.org/10.1016/j.niox.2020.01.007]
[http://dx.doi.org/10.1152/physrev.00044.2005] [PMID: 17237347]
[http://dx.doi.org/10.1042/CS20140361]
[http://dx.doi.org/10.1007/s00210-017-1379-y] [PMID: 28493050]
[http://dx.doi.org/10.1073/pnas.081082098] [PMID: 11287661]
[http://dx.doi.org/10.1002/med.21257] [PMID: 22549716]
[http://dx.doi.org/10.1371/journal.ppat.1004566] [PMID: 25521078]
[PMID: 26116588]
[http://dx.doi.org/10.2174/1570163812666150716111821] [PMID: 26264075]
[http://dx.doi.org/10.1002/art.23986] [PMID: 18975348]
[http://dx.doi.org/10.3389/fphar.2020.615598] [PMID: 33519481]
[http://dx.doi.org/10.1002/jbt.22888] [PMID: 34392583]
[http://dx.doi.org/10.1016/j.fct.2021.112604]
[http://dx.doi.org/10.1016/j.ijbiomac.2014.01.001] [PMID: 24412154]
[http://dx.doi.org/10.5306/wjco.v12.i5.342] [PMID: 34131566]
[http://dx.doi.org/10.1016/j.phrs.2004.06.002] [PMID: 15629256]
[http://dx.doi.org/10.3109/0886022X.2015.1103601] [PMID: 26513487]
[http://dx.doi.org/10.1016/0009-8981(72)90432-9]
[http://dx.doi.org/10.1136/jcp.13.2.156] [PMID: 13821779]
[http://dx.doi.org/10.1136/bmj.4.5839.552-e] [PMID: 4642815]
[http://dx.doi.org/10.1073/pnas.76.9.4350] [PMID: 388439]
[http://dx.doi.org/10.1016/0003-2697(78)90342-1] [PMID: 655387]
[http://dx.doi.org/10.1016/0014-5793(71)80319-8] [PMID: 11945853]
[http://dx.doi.org/10.1016/j.ejphar.2017.04.026] [PMID: 28438648]
[http://dx.doi.org/10.2337/db11-0807] [PMID: 22025779]
[http://dx.doi.org/10.1159/000520280] [PMID: 34673653]
[http://dx.doi.org/10.1016/j.ejphar.2018.10.035] [PMID: 30393200]
[PMID: 27383323]
[http://dx.doi.org/10.1007/s10735-009-9220-7] [PMID: 19484499]
[http://dx.doi.org/10.1038/s41580-020-0230-3] [PMID: 32231263]
[http://dx.doi.org/10.1152/ajprenal.00511.2012] [PMID: 23389458]
[http://dx.doi.org/10.18388/abp.2002_3812] [PMID: 12362995]
[http://dx.doi.org/10.1007/s12663-013-0599-z] [PMID: 25729233]
[http://dx.doi.org/10.1161/HYPERTENSIONAHA.111.185744] [PMID: 22215708]
[http://dx.doi.org/10.1097/HJH.0b013e32833366cd] [PMID: 19864959]
[http://dx.doi.org/10.4103/0253-7613.190744] [PMID: 27721541]
[http://dx.doi.org/10.1016/j.biotechadv.2017.12.015] [PMID: 29289692]
[http://dx.doi.org/10.1111/jcmm.15583] [PMID: 32628815]
[http://dx.doi.org/10.1080/03602530600971974] [PMID: 17145701]
[http://dx.doi.org/10.2337/db09-1342] [PMID: 20103708]
[http://dx.doi.org/10.1016/j.cbi.2014.09.015] [PMID: 25268985]
[http://dx.doi.org/10.1021/acsomega.2c00028] [PMID: 35252727]
[http://dx.doi.org/10.1046/j.1523-1755.64.s86.12.x] [PMID: 12969130]
[http://dx.doi.org/10.1111/jphp.12067] [PMID: 23738727]
[http://dx.doi.org/10.1016/j.molcel.2007.04.021] [PMID: 17560373]
[http://dx.doi.org/10.1016/j.lfs.2007.08.018] [PMID: 17869312]
[http://dx.doi.org/10.1007/s12253-014-9801-y] [PMID: 24925218]
[http://dx.doi.org/10.1016/j.yexcr.2017.09.042] [PMID: 28986066]
[http://dx.doi.org/10.1016/j.freeradbiomed.2019.04.033] [PMID: 31059771]